A new wearable sensor from the University of Michigan will provide more accurate and continuous fluid status data streams.
A team of University of Michigan researchers have developed a wearable sensor that could one day provide doctors with a simple, portable and completely non-invasive way to measure fluid status — the volume of blood that’s traveling through a patient’s blood vessels at any given time.
This sensor could perhaps be the answer to an age-old problem that has perplexed physicians, which is how to precisely determine the right circulatory volume is for an individual. Fluid status is a diagnostic measure much like heart rate or blood pressure. It can alert doctors when a cardiac patient has excess fluid that prevents their heart from pumping efficiently or provide a more precise measure of how much waste fluid to filter out of a dialysis patient’s blood. Additionally, it can tell a medical staff how much fluid to give to a trauma patient who has lost blood or a septic patient with an overwhelming infection.
At the moment, though, getting an accurate measure of fluid status requires an ultrasound or the insertion of a specialized catheter that measures the pressure of blood flowing through a blood vessel. Both tests are expensive and complex, and must be administered in a hospital by an expert. University of Michigan’s wearable sensor could change that by making measuring fluid status as simple as strapping a smartphone-sized device to a patient’s arm or leg and asking them to take a deep breath. And because it can be worn for extended periods of time, the unit could provide doctors and caregivers with an unprecedented amount of real-time data about fluid status.
The device works uses a process called Dynamic Respiratory Impedance Volume Evaluation, also known as DRIVE, to measure the changes in “bioimpedance,” or electrical conductivity, of the wearer’s limb as they breathe. Blood is an excellent conductor of electricity, so a patient with more blood will have greater conductivity. It’s quite similar to the ultrasound method of measuring fluid status, which directly captures the changes in the vena cava, the body’s largest vein. But instead of using the vein size to calculate fluid status, the new device gets the same information by measuring bioimpedance. While they may not be the first ones to use approach, the team is the first to incorporate fluid status measurement into a wearable gadget.
“You can absolutely, with DRIVE, track how much circulating volume someone has by taking this new vital sign and combining it with the treatment outcomes we expect. We can use it as a new way of honing in on where we want a patient to be and where are they currently,” says Barry Belmont, a biomedical engineering doctoral student at the University of Michigan.
According to Belmont, the new sensor is easy to use and requires minimal expertise, making it an ideal option for the intensive car unit, a small clinic, an ambulance, in an accident scene or even on the battlefield.
What’s more, the researchers say their technology could effectively make fluid status another vital sign. Current measurements like heart rate and blood pressure are diagnostic measurements that have been in place for decades or more. However, these methods don’t accurately address issue that patients experiencing trauma, undergoing dialysis, or septic patients commonly have in that they can’t capture the amount of blood flowing through a patient’s blood vessels.
“This could turn fluid status into a routine diagnostic tool, the way we measure heart rate and blood pressure today,” reveals Kevin Ward, executive director of the UM Center for Integrative Research in Critical Care (MCIRCC). “It has the potential to improve care and lower costs for millions of patients, and I think it’s a great example of how collaboration between fields like engineering and medicine can have a direct benefit on the lives of patients.”
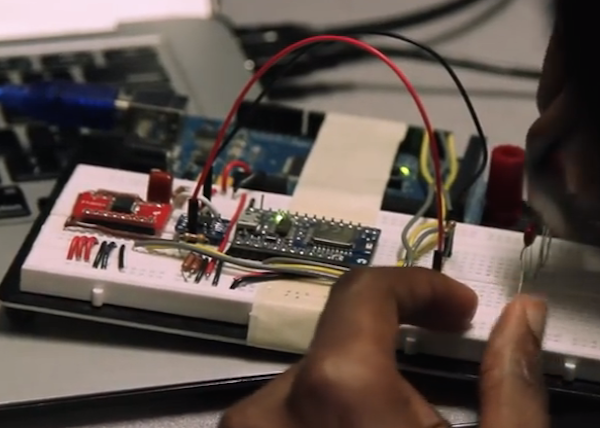
The team has been testing a benchtop version of the sensor, built from off-the-shelf components, for more than a year. At the heart of the wearable itself lies an ATmega1280 MCU, while an Arduino Mega was employed for much of the benchtop validation process. The systems works by sending small amount of electcricity around the limb. As it moves through the limb, the current either travels faster or slower based on the amount of blood volume. This actually enables them to count the number of respirations and how deep a wearer is breathing.
A real-time stream of fluid status data could even help doctors provide better treatment to patients who need additional fluid, like sepsis patients. The researchers predict their current round of testing will continue through the end of this year. If the trials are successful, the device will go to the FDA for approval.
“We’ve gone from something that’s fairly large with a comptuer and a tabletop to something that resembles a Nano iPod that you can wear on your arm,” Ward explains.
Intrigued? Head over to the University of Michigan’s official page to learn more, or listen to a more elaborate overview of the project in the video below!